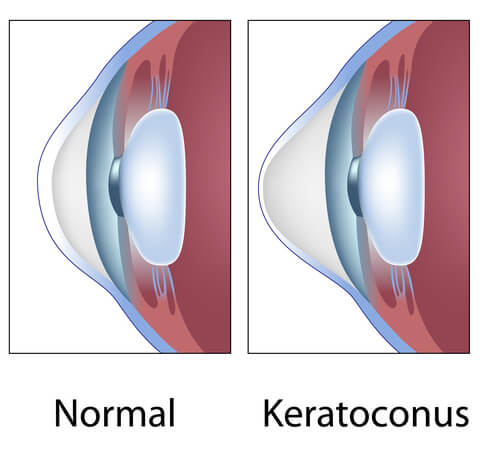
Keratoconus is a chronic degenerative disease affecting the cornea or the clear window in the front of the eye. While a normal cornea is usually spherical, like a basketball, a keratoconus cornea is distorted and cone-shaped. The distorted cornea leads to poor vision, and difficulty correcting the vision with glasses or contact lenses.
Keratoconus is often diagnosed during the teens and twenties and progresses throughout life. The cornea becomes progressively steeper, more distorted, and thinner. This typically leads to worsening of vision and the need for hard contact lenses. If not treated, keratoconus often leads to the eventual need for a corneal transplant. While a corneal transplant may be very effective, it is also very invasive. It may take months to even years before the best vision is attained. It also may require the use of eye drops indefinitely.
Patients with keratoconus often have chronic allergies and frequently report significant eye itching. They have a tendency to rub their eyes aggressively, which may lead to the progression of the corneal distortion. While the progression of the disease tends to slow down later in life, patients who are diagnosed in their teens and twenties tend to progress very rapidly.
Until recently, there was no effective treatment available in the U.S. to stop the progression of keratoconus. In the spring of 2016, corneal collagen crosslinking was approved by the FDA, and is now available in the U.S. Corneal collagen crosslinking involves treating the cornea with eye drops containing riboflavin, a B-vitamin. Once the cornea has been saturated with the riboflavin, the cornea is then treated with ultraviolet light. The light combined with the riboflavin leads to the formation of crosslinks, which are bonds within the cornea. These bonds provide strength to the cornea to make it more rigid and less susceptible to further weakening, thinning, and distortion. Not only has this treatment been shown to be effective at stopping the progression of keratoconus, but it has also shown that it can actually reverse some of the distortion already caused by keratoconus.
Corneal collagen crosslinking has been used internationally for many years. At Comprehensive EyeCare of Central Ohio, Dr. Kenneth Beckman was a principal investigator in two FDA trials since 2013 to help gain FDA approval for this treatment. Dr. Beckman has extensive experience in corneal collagen crosslinking and performed the first FDA- approved treatment in Ohio.
Patients with astigmatism, or an irregular curvature to the cornea, may need to be evaluated for keratoconus, using a corneal mapping test known as topography. Corneal topography is critical in making the diagnosis of keratoconus. Since corneal collagen crosslinking is most effective at preventing progressing, it is important that patients address this condition as soon after diagnosis as possible. If you have been told that you have astigmatism, or have had trouble attaining good vision in glasses or contacts, you may need an evaluation for keratoconus. Please contact Comprehensive EyeCare for a detailed evaluation.
